
A recent visit to a local hospital provided some insight on a particular problem in health care. After speaking to a few healthcare professionals, it was revealed that patients who have surgery are at a significantly higher risk at developing a Pulmonary Embolism (PE) as a result of a Deep Vein Thrombosis (DVT) or blood clot. Clots are also referred to as a thrombus. However, once a clot begins to travel it is called an embolus. You may have heard of these terms in the context of the myriad of commercials about blood-thinning medications. DVTs typically originate in the legs or arms and are associated with clots that are formed in the venous system. These clots are associated with either a genetic disorder, surgery or pre-disposition as a result of the nature of a disease. In particular, cancer patients are at higher risk for developing PEs.
Effects: The effects of these clots can be devastating to patients depending on their size. In theory, if the patient experiences a DVT in a leg or arm, the clot then travels through their veins, passing through the right side of the heart and lodges itself into their lungs. We won’t get into the details of the physiology of the lungs but suffice it to say that if the clot is large enough, it can shut down an entire lung and lead to death due to other complications. The other cases generally involve clots that are small enough to only effect smaller branches of the bronchioles. In this case, blocking smaller portions of the lung from oxygenating blood via the alveoli can result in problems breathing. In summary, clots can lead to death, quickly. In less severe cases, patients can have trouble breathing beyond what is considered normal variances. Having a pulse oximeter on-hand is great for detecting sustained oxygen levels below 90% saturation levels.
Diagnosis : Diagnosis of a DVT or PE can be performed via a Computer Tomography (CT) scan. These scans are typically the result of a patient complaining about a challenge with breathing, recent surgery, and/or a pulse oximeter reading that is consistently below 90%. These factors are not meant to be an exhaustive list, but rather an example of the types of cases that lead to indications of a deeper problem. In order to identify whether the PE resulted from a DVT, an ultrasound examination can be performed to determine the precise location of a clot.
Treatment : So how do medical professionals deal with patients with DVTs and PEs? The standard procedure is to immediately place the patient on a Heparin drip intravenously (IV) in order to reduce the risk of the clotting by monitoring various parameters. Heparin is used in this manner due to its fast-acting properties of blood-thinning. In more severe cases, lovinox shots are administered subcutaneously in the midsection when time is of the essence. Once a patient has achieved a status of therapeutic in both the International Normalized Time (INR) or Prothrombin Time (PT) and the Partial Thromboplastin Time (PTT), a transition to Warfarin (Coumadin) can occur. An INR reading of 1 indicates an average person‘s clotting time. An ideal INR value for patients who have experienced a PE is between 2 and 3. One can think of this as a patient taking 2–3 times longer for their blood to clot.
Physiology of Clotting : Blood consist of red blood cells (RBCs), white blood cells (WBCs), plasma and platelets. Over half of the total content of blood is plasma. RBCs make up 40–45% volume of blood. One measure of this volume is called the haematocrit count. Blood coagulation begins when the blood platelets are activated. Activation of platelets can happen by breaking the walls of a blood vessel, which releases specific chemicals in the endothelium layer. Another alternative for activation to occur is by prolonged exposure to a rapid increase in shear stress that leads to platelets being damaged. The release of these chemicals into the endothelium layer triggers what’s known as the Coagulation Cascade. The cascade can be best described as a series of positive and negative feedback reactions. The ending result of these reactions is the conversion of fibrinogen to fibrin. Fibrin strands then link together with the activated platelets to form a cross-linked fibrin clot. The details of this process including clotting factors is shown below.
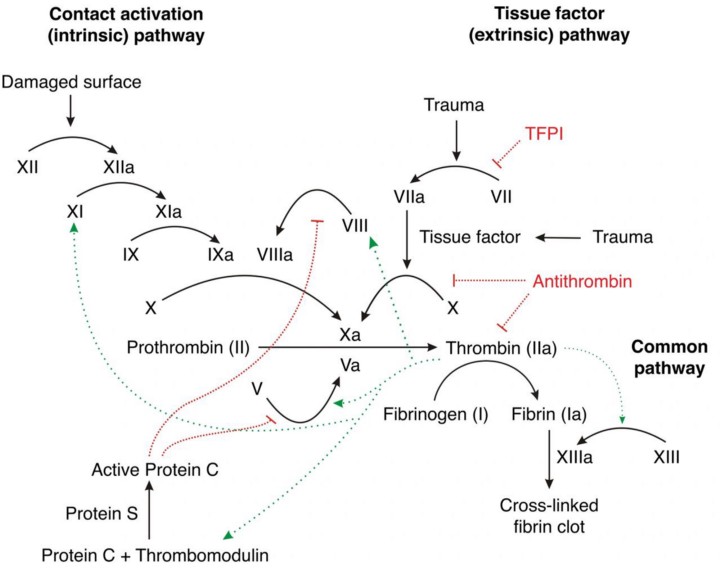
There are over 20 clotting factors involved in the process of blood clotting. Our liver is responsible for the production of various proteins which are involved with the clotting process. Vitamin K is an essential element in the clotting factors II, VII, IX, and X and anti-coagulant proteins C&S. Of the 20 or so clotting factors, the PTT and the INR are the two blood tests which indicate the presence of certain clotting factors. Normal PTT times range from 30 to 50 seconds and indicate the presence of the following coagulation factors: I, II, V, VIII, IX, X, XI and XII. Factors VII and XIII cannot be detected with the PTT test.
The Challenge: The rate at which the body metabolizes various foods containing vitamin K determines the INR readings. Foods that are high in vitamin K reverse the effect of warfarin, thus reducing the INR readings. As a result, being consistent with your intake of vitamin K is crucial in stabilizing the INR readings. Stability of the INR is achieved when subsequent blood tests are consistently in range. If INR readings are out of range, an anti-coagulation pharmacist then has the responsibility of immediately recommending a dosage adjustment based upon a dosage chart.
Anti-biotics also have an affect on INR readings. The website: Contemporary Clinic states that Warfarin is metabolized by the cytochrome (CYP) P450 enzyme system, specifically, CYPs 1A2, 3A4, and 2C9.2. Medications that inhibit these CYP enzymes reduce warfarin’s metabolism, increasing its effect, and increase INR. Medications that induce these CYP enzymes increase warfarin’s metabolism, decreasing its therapeutic effect, and decrease INR. Medications can also directly affect the clotting cascade, induce warfarin’s metabolism, or affect its protein binding. Warfarin is highly protein bound. If other medications displace warfarin on protein-binding sites, the free concentration will increase, creating a bleeding risk.
Antibiotics in the same class have similar effects on INR:
- Cephalosporins may increase INR by inhibiting production of vitamin K-dependent clotting factors.6,13
- Fluoroquinolones may increase INR by inhibiting warfarin metabolism, displacing warfarin from protein-binding sites, or disturbing intestinal flora that synthesizes vitamin K.7,13
- Isoniazid may increase INR by inhibiting warfarin’s metabolism.9,13
- Macrolides and metronidazole may increase INR by inhibiting warfarin’s metabolism.4,8,13
- Penicillin may increase bleeding risk by inhibiting platelet function.12,13
- Rifampin may decrease INR by inducing warfarin’s metabolism.10,13
- Sulfonamides may increase INR by inhibiting warfarin metabolism, displacing warfarin from protein-binding sites, or disturbing intestinal flora that synthesizes vitamin K.5,13
- Tetracyclines increase INR by an unknown mechanism, potentially inhibiting warfarin metabolism and plasma prothrombin activity.11,13
Conclusion: Blood clots are an extremely dangerous medical condition requiring a rapid response, blood thinning medication and constant monitoring by medical professionals. The patient’s role and responsibility in keeping their diet consistent, monitoring anti-biotic intake, taking blood-thinning medication on a timely basis, being regularly tested for their INR ranges, communicating with anti-coagulations pharmacists and subsequently adjusting their dosages is a tall order. Patients are required to be very organized in monitoring their own care. Clearly, those patients who lack organizational ability are at a disadvantage. Framing this problem as a positive feedback control system for INR values below 3.5 and as a negative feedback system for INR values greater than or equal to 3.5 makes sense. The only limitation is that there is currently no portable test for the INR and PTT measures akin to the blood-glucose monitors for diabetes patients that are available over the counter.
